Key Takeaways
AI predictive analytics reduces hospital readmissions by 10-20% and achieves 87% accuracy in early disease detection.
Personalized medicine with AI creates customized treatment plans based on genetic data, lifestyle factors, and medical history.
AI compresses drug discovery timelines from 12-18 years to 3-5 years, reducing costs from $2.6 billion per drug.
Remote monitoring through AI-powered wearables detects cardiac issues and predicts complications before symptoms become severe.
AI optimizes healthcare costs by improving staff scheduling by 15-20%, increasing surgical capacity by 10-15%, and reducing waste by 20-30%.
Why Predictive Analytics Matters in Modern Healthcare
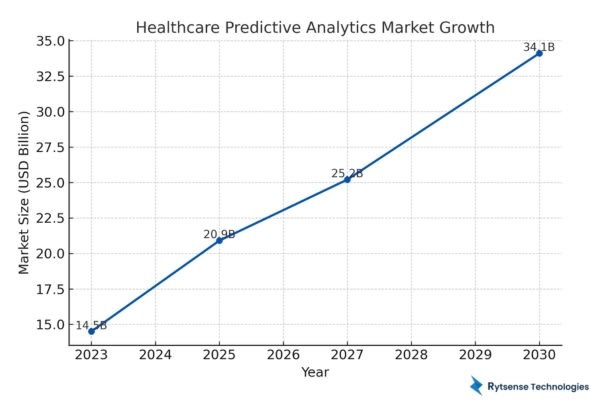
AI predictive analytics is transforming medical practice with information-driven predictive analytics for healthcare decision making. The global outlook for healthcare predictive analytics is expected to be a market valued at $34.1 billion by 2030, with a compound annual growth rate (CAGR) of 20.4%.
Study shows predictive analytics has lessen hospital readmissions by 10-20%, and even diagnostic systems with the use of AI show an 87% accuracy rate in early detection of diseases. These statistics demonstrate the benefit of AI and predictive analytics relating to patient treatment outcomes and operational effectiveness.
Healthcare organizations are looking for solutions in managing chronic disease, older populations, and lack of skilled providers. With the use of AI predictive analytics, healthcare organizations are able to analyze electronic health records, genomic and genetic data, clinical imaging, and real-time monitoring of patient disease progression and treatment protocols.
Defining AI Predictive Analytics in Healthcare
AI predictive analytics in healthcare applies machine learning algorithms to take meaning from clinical data. The technology analyzes associated patterns within patient records to uncover risk factors, generate disease onset predictions, and suggest potential treatment options.
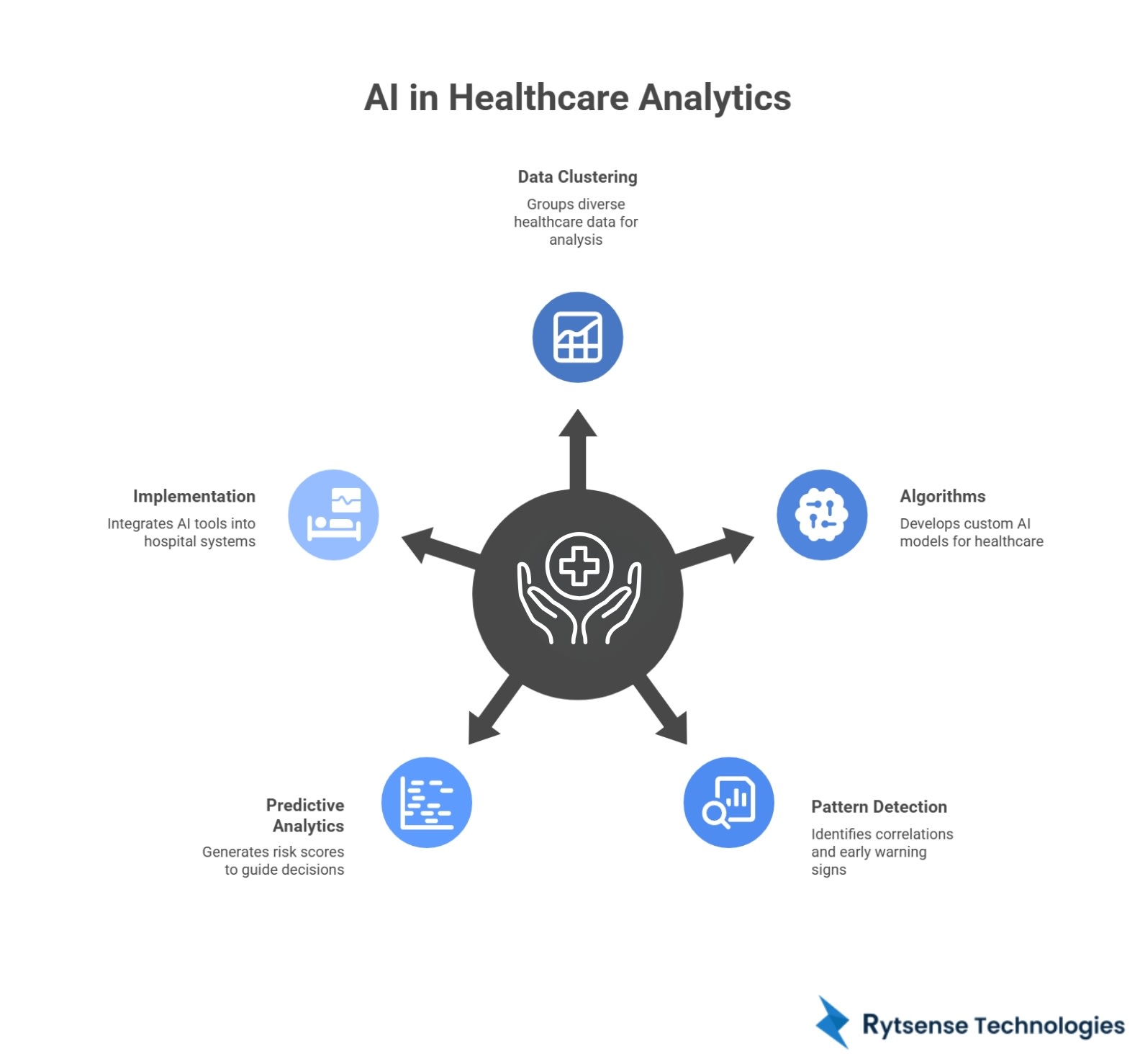
Four Basic Components:
- Data Clustering: Healthcare predictive models group data from clinical electronic health records, laboratory results, medical imaging data, wearable sensors, and/or genomic databases.
- Algorithms: Custom AI development firms build any number of customized neural networks, decision trees, and deep learning models. These algorithms derive relationships between variables.
- Pattern Detection: AI in healthcare analytics develops correlations across data sets. For example, these algorithms detect early warning signs for disease and predict responses to treatments.
- Predictive Analytics: Healthcare predictive models produce predictive risk scores which guide clinical decision-making. Whenever additional data is fed into the model, the model improves accuracy.
- Implementation: Predictive biomedical analytics technology and collaborate with hospital systems, and offer real-time analysis via dashboards, alerts, and notifications.
The Influence of AI on Predictive Analytics in Healthcare
The predictive abilities of artificial intelligence in health care have grown quickly. AI has the ability to take thousands of data points simultaneously and recognize patterns. This capability allows physicians and other health specialists to alter routine medical practice.
Improved Diagnostics: AI in medical analytics so that diseases can be detected earlier. For example, machine learning has been used to predict the result of imagining 95% of the time with dermatology cancers and outperformed human radiologists.
Faster Development: As a result of AI capabilities, the time for developing medications has been significantly decreased. By using AI in drug discovery, scientists are able to virtually screen hundreds of millions of compounds which significantly lowers the cost of research.
Population Health: AI predictive epidemiology assists with better understanding, predicting, and controlling disease outbreaks and vaccination strategies. For example, predictive models have been utilized to monitor the rate of infection of COVID-19 and predict hospital surges.
Operational Effectiveness: Improvements in the cost of health care have been extended beyond patient care; AI is supporting operational effectiveness in administration. Predictive models are used to estimate patient volumes, staff needs effectively, and optimize inventory supply chains.
Personalized Care: Personalized medicine with AI incorporates a person's genetic information, family history and lifestyle to develop customized treatments so that they make the best use of the therapy.
Ready to build intelligent predictive models for diagnosis, treatment, and patient monitoring?
Our AI experts help you design secure, accurate, and scalable healthcare analytics solutions.
8 Practical Use Cases of AI Predictive Analytics in Healthcare
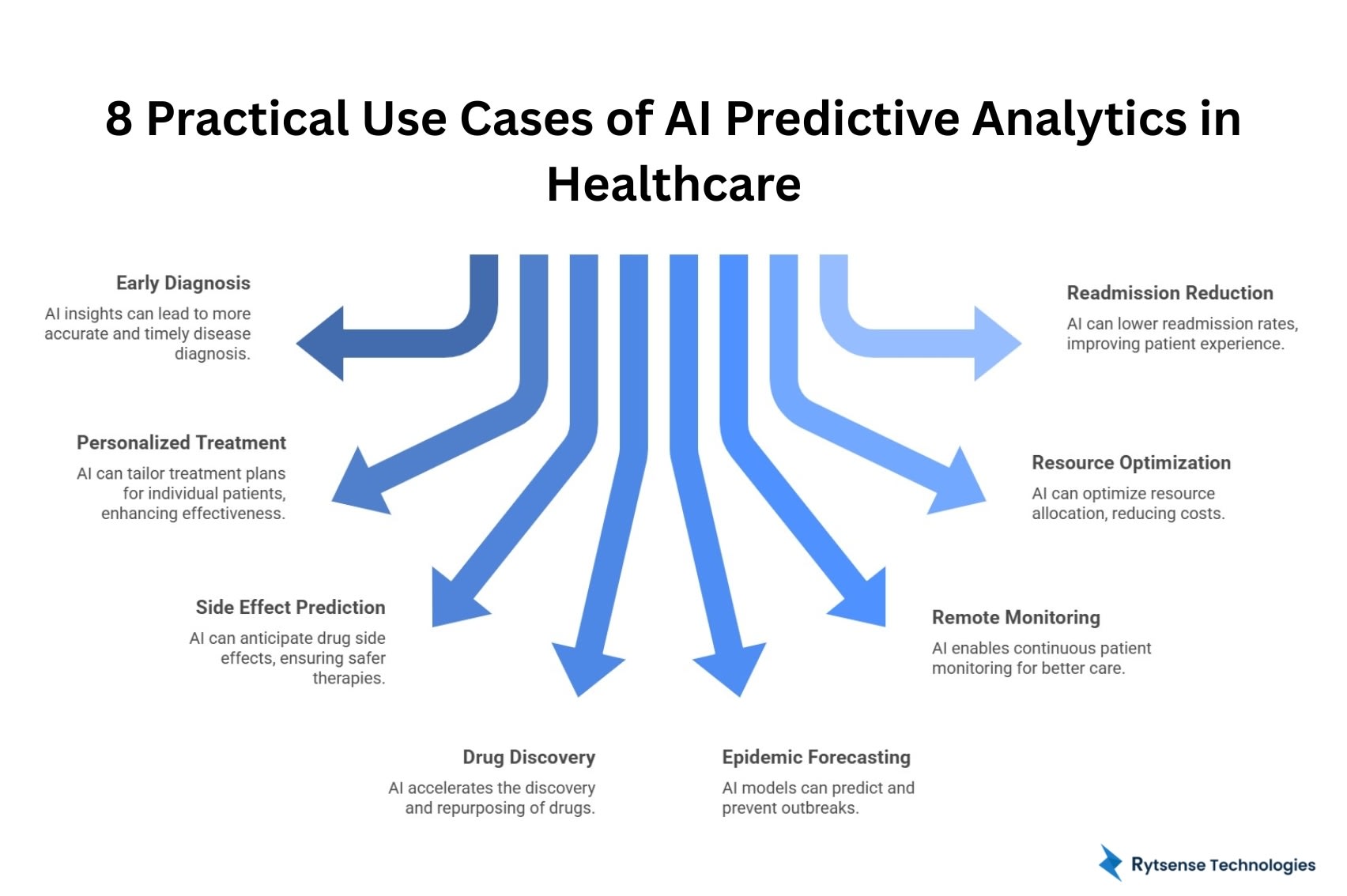
Early and Accurate Disease Diagnosis with AI Insights
Leveraging AI for patient satisfaction improvement to disease identification in oncology, neurology, and cardiology. AI systems integrate information derived from pathology, radiology, genomics, and clinical history to optimize diagnoses and identify potential in a timely manner.
In cancer care analysis, algorithms intelligently synthesize information derived from pathology biopsies and imaging, as well as genetic markers that can predict not only whether or not malignancy is likely but also the likely growth pattern. By examining hundreds or thousands of features of individual cells, aggressive disease characteristics can be detected. In breast cancer care, for example, higher specificity versus false negative rates reduction by 9.4% and 5.7% respectively.
Regarding Alzheimer's care, AI predictive analytics in healthcare applied to brain imaging and biomarkers can be executed years ahead of patient symptoms related to neurodegeneration, creating means for early intervention before symptoms exhibit.
IV Valyerna directed voice of Cortel ai care, wearables AI algorithms are predictive of heart rhythm changes and occur prior to heart failure and arrhythmias reports. Atrial fibrillation is an arrhythmia determined by AI using cloud-based wearables in the ambulatory setting for population screening the over age of 65.
Implementation:
- Integrated with PACS
- Real-time analysis of image scans with automatic alerts and alarms issued upon outlining the data
- Implemented clinical care support at the workstation of the ordering physician
- Continuous improvements for the model to work for high runtime issues.
Personalized Treatment Plans and Precision Medicine
The emergence of customized medicine that utilizes artificial intelligence (AI) has ushered in a new era of customized treatment strategies. Genetic variation dictates that even identical therapeutics will yield different clinical outcomes in different patients. AI-powered treatment plans will examine an individual patient's genomic sequences, protein expression patterns, metabolic features, and microbiome composition, thereby rendering a more precise match of patients to the most appropriate therapy.
For example, in oncology, tumor genomic profiling has enabled oncologists to identify genomic mutations that drive tumor growth. AI systems to assign molecular signatures to targeted therapies will transform treatment for advanced melanoma, lung cancer, and leukemia.
Another example involves diabetes management. Now, there are diabetes platforms that combine real-time glucose monitoring with dietary logging, activity logging, and medications. AI technology can, in real time, provide recommendations for insulin dosing, while learning each individual patient's physiological response to various recommended changes.
Lastly, pharmacogenomic testing, coupled with AI prescribing systems reduces the occurrence of negative medication reactions. As an example, prior to prescribing a potentially harmful medication, the clinician can consult the AI system to identify the likely effect, dosage, and timing for their patient and its effectiveness based on their individual genomic/phenotypic data.
Anticipating Drug Side Effects for Safer Therapies
Consider the hazard of adverse effects from drug therapy, predicting drug-related adverse reactions can help reduce risk. Adverse drug reactions are listed among the most common causes of death in the United States, accounting for 100,000 deaths each year. AI-based systems for predicting adverse events prior to their occurrence.
Machine learning in healthcare models utilize input data about the molecular interactions between a drug and the patient protein or proteins targeted by the drug. For example, at Arizona State University, researchers created a predictive AI model to anticipate what impact a drug would have on the human immune response by focusing on molecules called MHC-1 proteins.
Polypharmacy can lead to additional risks due to drug-drug interactions. Elderly patients taking several medications are especially at risk for multiple adverse events. AI models predict drug-drug interactions to identify the most concerning combinations.
For example, a hypertension patient taking hydrochlorothiazide who becomes dehydrated, could be assessed using an AI comparative analysis of alternative medications. For example, the AI model may predict that use of an ARB would control the patient's blood pressure without adverse events.
AI will also help identify patients who are at risk for rare adverse events. Prior to prescribing a cardiotoxic chemotherapeutic agent, oncologists would consult the AI system that would assess a patient's risk based on that patient's cardiac history and any pertinent genetic history.
Faster Drug Discovery and Repurposing Through AI
AI can condense the development timeframe in drug discovery from 12-18 years to 3-5 years, which can also result in costs dropping from $2.6 billion per drug.
Generative AI in the pharmaceutical industry enables scanning of chemical libraries that have millions of compounds and predicting which compounds will bind with disease targets. In the past, discoveries relied on physically screening thousands of compounds. AI, however, can simulate virtual experiments in advance and better narrow the candidates that will be synthesized.
The technology then analyzes the structure of the molecules and predicts the binding affinity, pharmacokinetics, and toxicity profile of discovered or designed molecules.
Drug repurposing refers to attempts to re-purpose existing drugs for new indications. AI can analyze the molecular mechanisms of actions for drugs that have been previously authorized by the FDA to determine if there are therapeutic benefits for other conditions. For example, an approved drug for the treatment of rheumatoid arthritis may also show efficacy in treatment of an autoimmune condition affecting the skin. This can lead to expedited clinical trials for established, FDA approved drugs.
The public response to vaccine development to address COVID-19 serves as a case study for showcasing the application of AI in reducing drug development timelines. During this time, researchers utilized predictive modeling to inform the design of mRNA and evaluate the optimization of the formulation to enable the development of the vaccine in less than one year.
AI Workflow:
- potential targets identified based on assessment of the disease biology
- virtual screening of millions of molecules
- lead optimization to determine if it is efficacious and safe
- prediction of toxicity and safety profiles prior to human clinical trials
- design of human clinical trials to optimize success
Epidemic Forecasting and Outbreak Prevention with AI Models
AI-enabled epidemiology is transforming public health from a responsive management approach to a proactive prevention approach. Models combine disease surveillance with climate data, migration patterns, social media utilization, and search activity, allowing for the forecasting of disease outbreaks.
The University of Virginia's dashboard is a disease surveillance dashboard for enteric cousins, plotting areas of transmission, and outbreaks based on rainfall and sanitation, population density, and local historical information to identify afflicted communities.
Dengue fever forecasting overlays historical case data with rainfall, temperature, mosquito cycling, travel data, and searches for dengue symptoms. AI systems, through collected data, can alert authorities days and weeks before clinical cases appear, enabling mosquito control services and hospital preparedness.
Natural language processing monitoring from social media updates and news-cycle events can also be done, in real time. When there was Ebola outbreak in 2014, AI systems monitored conditions and detected patterns of spread days before confirmation from World Health Organization testing.
Climate change will continue to challenge the emergence and re-emergence of infectious diseases. AI models can examine and project how temperature shifts the patterns of transmission to enable proactive approaches.
Emerging remote healthcare monitoring of unusual symptoms of syndromes (e.g., spike in fever, respiratory distress) can alert authorities to outbreaks before patients present for medical care.
Remote Patient Monitoring for Continuous Care
Remote monitoring of patients allows for continuous monitoring outside of clinical space. Wearable devices can get heart rate, blood pressure, oxygen saturation, and activity levels. AI algorithms can detect dangerous changes in these values.
Cardiac monitoring provides clear life-saving potential. Wearable ECG sensors observe, check and analyze heart rhythm, detecting atrial fibrillation that increases the risk for stroke. AI continuously monitors the patient, collecting information and documenting transient observations to justify anticoagulation therapy.
AI to improve patient satisfaction is not limited solely to medical monitoring. Systems now monitor medication adherence and alert caregivers if activity decreases to a certain amount, indicating an increased risk for falls.
Post-surgical monitoring utilizes sensors that indicate wound healing, certain vital signs, and pain. AI monitoring allows for early event complication indications such as infection or blood clots. This is important to provide timely intervention before the complications become emergencies.
Patients with heart failure have access to smart scales, where signals can indicate rapid weight gain associated with fluid retention. AI is able to predict decompensation events several days prior to acute and severe indications. The patient would have sufficient time to preemptively manage increased diuretics.
Diabetes platforms utilize continuous glucose monitors transmitting glycemic readings to AI systems. Through time, these technologies allow the patient to maintain the optimum glycemic state with real-time advice from AI.
Technologies:
- Wearable ECG monitors
- Continuous glucose systems
- Smart medication dispensers
- Activity trackers
- Connected blood pressure monitors
- Sleep analysis devices
Optimizing Healthcare Resources and Reducing Costs
Cost optimization in healthcare using AI is a response to fiscal pressure. AI predictive analytics in healthcare upgrades allocation, minimizes waste, and increases efficiency without sacrificing care.
Patient flow prediction estimates volume metrics for admissions, emergency department usage, and surgical loads, dependent on patterns, trends, and even weather. Hospitals may use this to optimize staff scheduling to ensure coverage during peak hours to avoid overtime pay.
Surgical suite optimization maximizes operating room capacity. Predictive models estimate the duration of cases based on the procedure and surgeon originating patterns. Algorithms schedule cases with the intent of minimizing idle time, allowing for increased volume without having to add additional operating rooms.
Supply chain management predictions for medication, contraptions, and teaching supplies represent another area of potential application. Hospitals maintain large inventories of medical products, however storing excessive quantities of some items ties up capital in additional supplies. AI products trigger supply buys based simply upon utilization patterns.
ED congestion can cause troublesome situations. AI can be used to anticipate surge pattern usage allowing hospitals to take further proactive measures such as to call in additional staff to address increased workload, or more profoundly, open another observation unit prior to cases.
Billing AI healthcare applications are now on the market for denoting coding issues, and denial risk. AI products can analyze documentation and comment on deficiencies or potential codes that impact revenue.
Predictive maintenance of equipment improves continuity and prevents failure of critical equipment. AI can monitor devices such as imaging machines (e.g., CT and MRI), and analyzers as they operate, predictive data analysis in healthcare warranty patterns of degradation that fall short of a breakdown.
Lowering Readmission Rates and Enhancing Patient Experience
AI-based technologies to decrease hospitalizations address patient pain and expense. A readmission occurring within 30 days of discharge suggests inadequate discharge plans and aftercare protocols. Medicare penalizes hospitals with high readmission rates and in their claim processing establish penalties or disallow payment for excessive readmissions.
The literature indicates that current post-discharge readmission rates are 15.3%, with persistence of symptoms responsible for 43% of readmissions. AI predictive analytic tools in healthcare are being used to identify the patients most likely to be at risk for readmission prior to discharge.
Risk models can analyze past medical history, current hospitalization data, psychosocial history, current medications, and other relevant data points. Risk models will then provide the patient with readmission scores. While the determination of who qualifies as at-risk is subjective, these risk models generally identify patients as at-risk.
There is often increased value and satisfaction when patients receive personalized discharge instructions. AI termination can generate personalized discharge instructions in layperson's language, explaining medications and using pictorial presentations, with information about the medications and monitoring of symptoms.
As part of the post-discharge monitoring process, wearables can be utilized to monitor vital signs, signs and symptoms, and adherence. AI capable of detecting patterns of warning around increased blood pressure, reduced mobility, or missed doses can add valuable outreach before the patient becomes readmission eligible.
Many patients with chronic conditions will need ongoing management. AI-assisted technology can identify patients who require disease management services and education, including the monitoring necessary to keep them functioning, safe, and out of the hospital.
Whether you're a hospital, clinic, research lab, or pharma company—our team builds secure, compliant, and scalable AI solutions.
Things to Implement AI Predictive Analytics in Healthcare Systems
The advancement of AI predictive analytics in healthcare requires a formal process for implementation.
Assessment Process: Identify clinical and operational issues that can be solved through predictive analytics. Conduct a readiness assessment to analyze data infrastructure and capabilities. Prioritize use cases having an impact along with feasibility.
Data Infrastructure: Predictive models in healthcare require quality and comprehensive data. Implement governance frameworks to ensure integrity and quality. Combine all data sources (EHR, labs, imaging, billing) into a single warehouse.
Seller Partnering: Give engagement with AI development services/outside vendors that have experience in healthcare. Assess vendors based on relevant clinical expertise/industry knowledge, regulatory compliance, and support.
Pilot Implementation: Initially start with very small scope pilots that demonstrate immediate value. Pick sections of care delivery that have physician champions, measurable metrics, and reasonable complexity.
Clinical Integration: AI healthcare integration must fit into workflow without adding to burden. Engage in user-centered design discussions to incorporate the resulting predictions into the existing EHR interface. Provide clear and prompt explanation of treatment recommendations. And no recommendation should supersede the ability of the human to act and either accept or further investigate the prediction.
Training: Ideally this will be a comprehensive training program to create understanding of AI capabilities and limitations. Address issues such as the fear of AI replacing clinical judgment. Create feedback loops and adapt messaging where needed.
Regulatory: Ensure compliance with current HIPPA, FDA requirements, etc. and state requirements. Put Safety and appropriate security measures in place, along with specific documentation for validation and monitoring.
Ongoing Monitoring: AI needs ongoing performance monitoring such as prediction accuracy, clinical impact, adoption patterns, and patient outcomes. Implement a continuous learning framework.
Scaling: Once piloted successfully, scale across clinical areas and sites. Develop implementation playbooks that capture lessons learned. Build internal data science teams.
Also Read:
AI in real estate development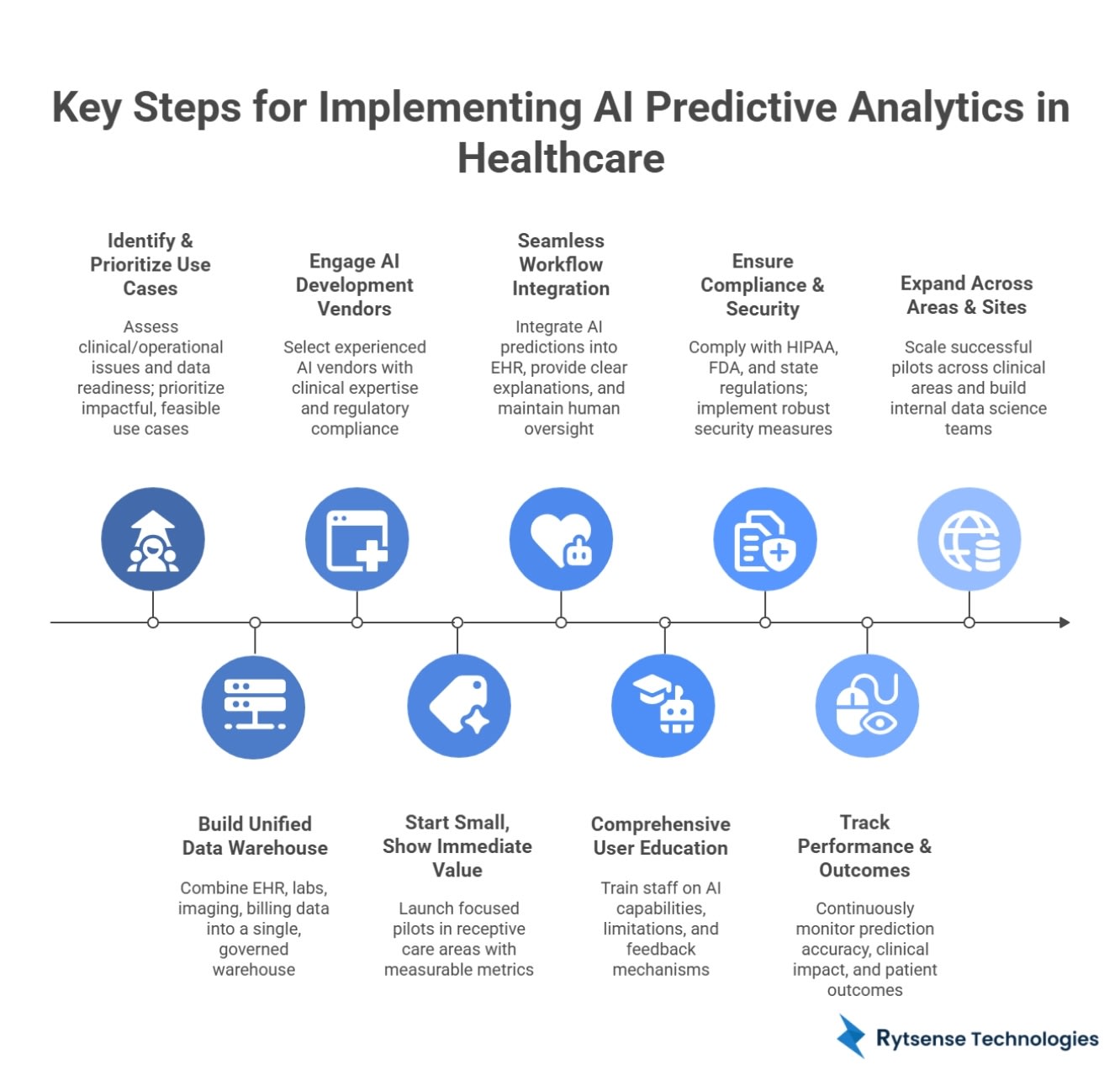
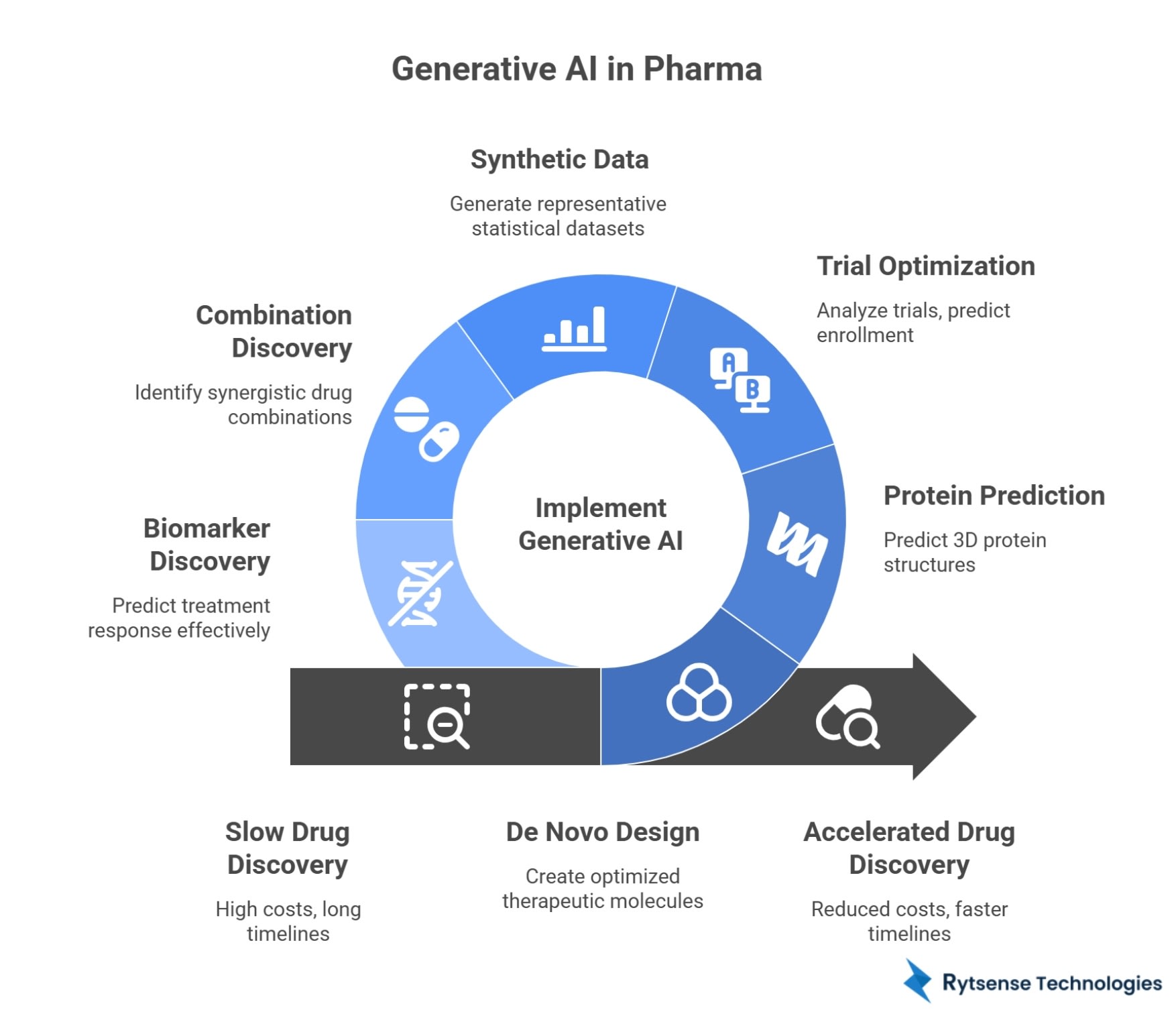
Generative AI in Pharma: Creative Real-World Applications
Generative AI in pharma can do quick drug discovery, optimize clinical trials, and personalize treatment development for patients. In drug design, generative AI can work to create new structures and generate hypotheses.
- De Novo Design: Generative models can design new molecules that are optimized for therapeutics. AI can generate new structures, literally from scratch, that have desired properties- binding very strongly, with good pharmacokinetics and low toxicity.
- Protein Prediction: AlphaFold is now able to predict 3-dimensional protein structures from protein sequences with atomic accuracy. Understanding structure is critical for drug design.
- Trial Optimization: Generative AI can optimize clinical trial protocols by analyzing successful previously conducted trials. The technology can identify the characteristics of patients, predict the time to enroll patients, and suggest adaptive designs for the trial.
- Synthetic Data: Privacy regulations may restrict access to patient data. Generative models can generate synthetic datasets that represent the statistical properties of real data, albeit not using real patient information.
- Combination Discovery: AI can efficiently explore drug space for combinations of drugs and identify synergy when multiple drugs are used together to elicit an outcome that is better than the sum of the individual medications.
- Biomarker Discovery: Generative AI can take genomic, proteomic and metabolomics data to identify novel biomarkers that will predict how well a patient will respond to a given treatment.
AI for pharmaceutical R&D will reach a total business investment of $3 billion by 2025. Early adopters in the pharma industry suggest that AI can lead to 40-50% reductions in discovery time, cost savings of greater than $1 billion per drug developed.
Conclusion
AI predictive analytics in healthcare allows for proactive prevention, tailored treatment, and effective delivery. Beginning with disease diagnosis, remote AI patient monitoring with AI-driven treatment program guidance, and making healthcare cost optimization using AI, these AI technologies are changing medical care. These include reducing hospital readmission with AI; rapidly transforming the drug discovery process with AI; and using AI in the implementation of action-oriented epidemiology to demonstrate quantifiable outcomes.
Healthcare organizations are positioning themselves at the forefront of innovation when they partner with an AI development service and/or custom AI development companies, enabling them to adopt predictive healthcare solutions. The application of machine learning in healthcare, predictive analytics tools for healthcare, and the use of AI predictive analytics in healthcare creates a future where care is predictive, personal, and precise.
Not sure where to start?
Get a step-by-step strategy tailored to your organization's needs.
Meet the Author

Karthikeyan
Connect on LinkedInCo-Founder, Rytsense Technologies
Karthik is the Co-Founder of Rytsense Technologies, where he leads cutting-edge projects at the intersection of Data Science and Generative AI. With nearly a decade of hands-on experience in data-driven innovation, he has helped businesses unlock value from complex data through advanced analytics, machine learning, and AI-powered solutions. Currently, his focus is on building next-generation Generative AI applications that are reshaping the way enterprises operate and scale. When not architecting AI systems, Karthik explores the evolving future of technology, where creativity meets intelligence.